Residents participate in clinical care, health promotion, and public health experiences at a variety of community health locations including United Community Clinics, the Mazzoni Center, local nursing homes and adult day care facilities, domestic violence shelter and transitional housing programs in Philadelphia, the Penn Medicine Hospice program, Unity Clinic, and other sites. We believe that this exposure is important in order to produce future physicians who recognize the powerful effects that environment and socioeconomic status have on health quality.
To be effective community-based providers, residents choosing to pursue careers in clinical medicine, basic science or academic/research-based careers need to be able to expand their perspective, be introduced community-based interventions, and translate their clinical and research knowledge to the bedside or community practices. In addition, in response to the health needs of the local community and region, resident awareness of health disparities and effective ways to work with communities to overcome community-based obstacles to healthy communities must be targeted. Increased exposure to an underserved, ethnic minority population may serve as a resource to help improve the health of our community while educating residents in community medicine and public health. We believe that our training program is a model for developing the next generation of primary care providers trained to mitigate health disparities and to serve as advocates for our community.
The community medicine curriculum takes place within a longitudinal program of didactics, community outreach, health promotional work at community sites, and work with the Philadelphia Department of Public Health. Residents rotate through a four-week block of community medicine in their PGY2 and PGY3 years.
Community medicine content included in the curriculum covers a diverse range of topics such as:
- Transportation
- community health
- health care safety net
- insurance (e.g. Medicaid, CHIP, Medicare)
- public assistance (e.g. TANF, SSDI)
- public housing
- child abuse/neglect
- elder abuse/neglect
- intimate partner violence/abuse
- community violence
- violence services
- in-home services for older adults
- long-term care of older adults
- care for the LGBTQ community
- harm reduction strategies
- refugee and immigrant health
- school-based health promotion and mentorship
- Patient Centered Medical Home and other progressive models of care (e.g. Federally Qualified Health Centers)
- mental health services
- occupational medicine
- communicable diseases
- environmental illness
- immunization strategies
- disease screening
- disease prevention
- health promotion
- health literacy
- social determinants of health
- epidemiology
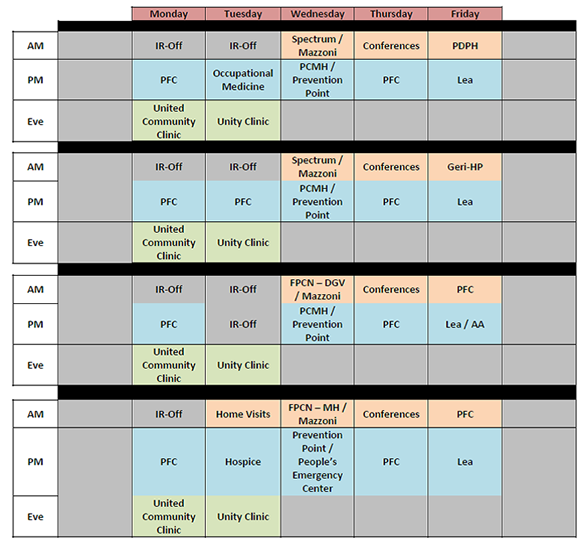
The table below describes the layout of elements of the experiential community medicine content of our curriculum.
Current Partners:
Free Clinics
Penn's Family Medicine residents help to support the operation of three free clinics during their community medicine rotations. Some residents choose to engage longitudinally with these sites using elective time.
- United Community Clinics
- Unity Clinic
- Philadelphia Department of Public Health
Community Medicine Didactic Lectures
Community medicine didactic lectures occur on the second Thursday of every four-week block. Community medicine content presented is designed to focus on skill-based sessions, providing practical content that can be used in the clinical encounter or in public health work addressing the healthcare needs of the underserved. Community medicine didactic content has included:
- Reach Out and Read
- Food Security/Policy
- Asian Immigrant Primary Care
- Hospice, Child Abuse
- End of Life Symptom Management (non-pain)
- Injury Prevention
- End of Life Pain Management
- Sexual Abuse
- Healthcare for the underserved
- Injury Prevention
- Primary care providers as policy advocates
- Epidemiology (Measures of Association)
- Immigrant Health, Epidemiology (RCTs)
- Disaster Preparedness
- Epidemiology (CBPR and Qualitative)
- Public Assistance
- Using Census data
- Domestic Violence – Victimization
- Drew Health Collaborative
- Epidemiology (IRB and Research Ethics)
- Community Schools
- Health Insurance and Medication Coverage
- Health Policy 101
- Services for the Elderly
- Epidemiology (Study Design)
- Health Literacy
- Family Care Giving
- Neighborhoods and Health
- Accessing Care
- Long-Term Care
- DFMCH Activities in Central America
- Primary care for the LGBTQ Community
- Disability
- Public Health GIS
- Epidemiology (Bias and Confounding)
- Epidemiology (RCTs: Practical Applications)




Home Visitation Program
Our Home Visitation Program is a model of multidisciplinary collaboration including Family Medicine faculty, residents, Social Work, and Pharmacy. Our indications for home visits include: Newborn Evaluation, Post-partum Evaluation, Home Hospice Care, Long-term Care Needs Assessment, Inpatient Discharge Transition, Poly-pharmacy, Medication Adherence Evaluation, Home Care Needs, Safety Assessment, and Insurance Counseling.
Home visitation is an opportunity for learners to share in the lived experience of their patients. For many learners, this is a formative experience: "I've always imagined that medical adherence is very challenging, but visiting a patient in their home helps me to understand  why and how they are unable to adhere. It also helps me to understand how I as a physician can help." Another resident commented: "I realized that a lot of patients downplay their needs or my perception of their living situation was completely inaccurate".
why and how they are unable to adhere. It also helps me to understand how I as a physician can help." Another resident commented: "I realized that a lot of patients downplay their needs or my perception of their living situation was completely inaccurate".
School-Based Collaboratives
DFMCH has worked in partnership with local schools in our service community for over a decade and a half with focused work starting at the K-8 grade Charles R. Drew School and more recently with the 9-12th grade University City High School (UCHS). Unfortunately our partnerships have been challenged with both schools being closed under the pressures of economic, academic, and social stressors affecting the ability of our local schools being able to meet the needs of our community youth. Resident physicians and faculty  have worked with students, teachers, and administrators on improving the health of our community and supporting sustainable support of community schools. We have begun a new partnership with the Lea K-8 elementary school and are developing and implementing a health promotion curriculum for Lea students focusing on health lifestyles and healthy relationships. Our partners include the Lea community, UPenn's Graduate School of Education, and the Center for Public Health Initiative's Service Link. Service Link's (Service Link) overall mission is to improve the health of low-income patients in Philadelphia by linking them with a variety of benefits that they have a right to attain under current US legislation. Service Link focuses on addressing the social determinants of health through education and community engagement.
have worked with students, teachers, and administrators on improving the health of our community and supporting sustainable support of community schools. We have begun a new partnership with the Lea K-8 elementary school and are developing and implementing a health promotion curriculum for Lea students focusing on health lifestyles and healthy relationships. Our partners include the Lea community, UPenn's Graduate School of Education, and the Center for Public Health Initiative's Service Link. Service Link's (Service Link) overall mission is to improve the health of low-income patients in Philadelphia by linking them with a variety of benefits that they have a right to attain under current US legislation. Service Link focuses on addressing the social determinants of health through education and community engagement.
Our curriculum focuses on:
- Body Image Awareness
- Nutrition/Exercise
- Normal Growth and Development
- Tobacco, Alcohol, and Drugs
- Peer Pressure, Violence Prevention, Safety, Conflict Resolution, toxic stress
- Hygiene
- Sexual Health, HIV/STI awareness and prevention
- Teen Parenting
- Chronic Health Conditions
- Periodic Health Maintenance
Contact Information:
Peter Cronholm, MD, MSCE
Director, Community Programs
Department of Family Medicine and Community Health
3400 Spruce Street
2 Gates Building
Philadelphia, PA 19104
Telephone: 215-615-0850