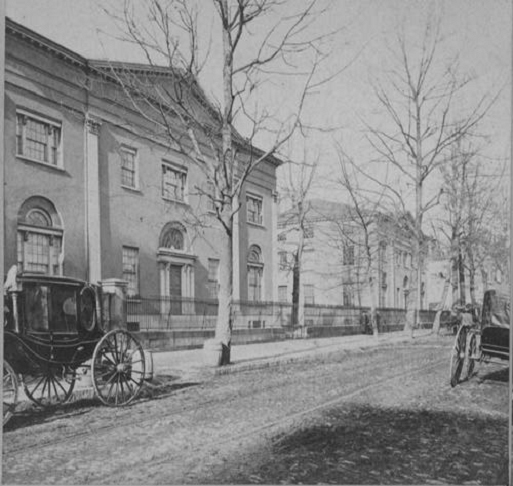
 Founded by Benjamin Franklin in 1740 as a charity school for Philadelphia children, the University of Pennsylvania was America's first university and one of its foremost institutions for teaching and research. The nation's first medical school, its first business school, the first journalism program, the first university teaching hospital, the first computer and the first modern liberal-arts curriculum were all established at Penn.
Founded by Benjamin Franklin in 1740 as a charity school for Philadelphia children, the University of Pennsylvania was America's first university and one of its foremost institutions for teaching and research. The nation's first medical school, its first business school, the first journalism program, the first university teaching hospital, the first computer and the first modern liberal-arts curriculum were all established at Penn.
The Perelman School of Medicine was the first and only medical school in the 13 American colonies, opening its doors to students in the fall of 1765. The founder of the School of Medicine was a young Philadelphia physician, John Morgan.
The early faculty, including Morgan, earned medical degrees at the University of Edinburgh and in advanced courses in London. With the University of Edinburgh as their model, they built the School of Medicine within an institution of higher learning. They emphasized the need to supplement medical lectures with bedside teaching.
For more than a century, the pattern of medical education remained relatively unchanged and the standards and procedures introduced by the University of Pennsylvania remained the guiding force in medical education.
 Philadelphia's history and the history of neurosurgery in America are often intertwined. It is not surprising that the impetus and intellectual base for the development of neurological surgery should arise in Philadelphia, arguably at the end of the 19th century, the epicenter of American neurology. Some of the leading neurologists, including S. Weir Mitchell (1829-1914), Charles K. Mills (1845-1931), and William Gibson Spiller (1863-1940), all worked within the neurology department of the University of Pennsylvania.
Philadelphia's history and the history of neurosurgery in America are often intertwined. It is not surprising that the impetus and intellectual base for the development of neurological surgery should arise in Philadelphia, arguably at the end of the 19th century, the epicenter of American neurology. Some of the leading neurologists, including S. Weir Mitchell (1829-1914), Charles K. Mills (1845-1931), and William Gibson Spiller (1863-1940), all worked within the neurology department of the University of Pennsylvania.
It was no accident, for example, that William W. Keen's first successful craniotomy for a brain tumor in 1887 occurred in the presence of Dr. Mitchell. Dr. Mills, regarded as "the dean of American neurologists" was the first to describe the syndrome of occlusion of the superior cerebellar artery. Dr. Spiller, one of the most distinguished neurologists of his time, became a pioneer in the field of vascular occlusions of the brain stem and worked closely with the pioneer surgeon Dr. Charles Harrison Frazier.
Indeed, it was Dr. Frazier (1870-1936) who played much the same pioneering role in neurosurgery in Philadelphia that Dr. Harvey Cushing played in Baltimore and later in Boston. Dr. Frazier was not only responsible for establishing a division of neurosurgery at the University of Pennsylvania, but also for inaugurating a "Philadelphia school" of neurosurgery, which later included Francis Grant, Temple Fay, Robert Groff, Frederick Murtagh, R. Michael Scott, Henry Shenkin and Thomas Langfitt.
The Legacy of Charles Harrison Frazier, MD
 Charles Harrison Frazier was born in Philadelphia on April 19, 1870. He did both his undergraduate and medical training at the University of Pennsylvania earning a BA in 1889 and a medical degree in 1892.
Charles Harrison Frazier was born in Philadelphia on April 19, 1870. He did both his undergraduate and medical training at the University of Pennsylvania earning a BA in 1889 and a medical degree in 1892.
After internships at the University of Pennsylvania and the Episcopal Hospital, he went to Europe to study surgery, neurology and pathology. There he trained under Professors Virchow and von Bergmann at the University of Berlin where he mastered aseptic technique.
Dr. Frazier started at Penn as an instructor in surgical pathology in 1896, and was elevated to clinical professor of surgery in 1901, a position he held with great distinction for some 15 years. In 1903, at age 33, he was appointed Dean of the Medical School and he served that post for 10 years. During his tenure as Dean, he was responsible for substantial academic strengthening of the institution, including raising entrance requirements and the introduction of new faculty trained at outside institutions.
Around 1908, Harvey Cushing and Dr. Frazier were considered to be the only two surgeons in the United States with extensive neurological practices. Frazier's decision in 1919 to devote himself almost exclusively to neurosurgery was influenced by his accomplishments as a military physician during World War I in Foxhills and Cape May. He reported on 500 cases of peripheral nerve injury and repair, as well as 200 cases of gun-shot wounds of the head. His interest in the surgical approach to intraspinal and intracranial tumors was stimulated by both Charles K. Mills and William G. Spiller, successive professors of neurology at the University of Pennsylvania.
Dr. Spiller's and Dr. Frazier's names have repeatedly been linked in numerous neurological treatments based on the former's research and the latter's surgical skill. For example, tic douloureux probably was described as early as Greco-Roman times. However, it was not until the late 19th century that the trigeminal nerve was implicated as the source of the pain.
At that time, surgeons resected the entire gasserian ganglion of the fifth nerve resulting in several postoperative complications including keratitis sicca and motor deficits (2). In 1901, Dr. Spiller showed that the sensory root of the gasserian ganglion did not regenerate after its fibers were transected.
Dr. Frazier furthered this observation by showing that retro resection of the ganglion was not only technically possible but easier than ganglionectomy. The Spiller-Frazier solution led to a safer intervention for trigeminal neuralgia. In the 700 or more cases of tic douloureux operated on by Dr. Frazier, the mortality rate was less than 0.5 percent, keratitis was minimal and motor deficits rare.
Drs. Spiller and Frazier are linked in the development of Dr. Spiller's idea to cure intractable pain by section of the anterolateral column of the spinal cord. From the 1880s, posterior rhizotomies were usually done but, according to Dr. Frazier, this gave relief to only 19 percent of the patients. This high failure rate was undoubtedly secondary to a lack of understanding of the pain tracts and functional anatomy of the spinal cord at that time.
Dr. Spiller provided understanding of the location of the pain fibers and suggested to Dr. Frazier that the neurosurgeon could relieve lower-body pain by severing the anterolateral tracts. Dr. Frazier was inherently skeptical and refused to attempt such an experimental operation. Instead, Edward Martin, John Rhea Barton Professor of Surgery at that time, performed this operation in 1911.
Three years later, Dr. Frazier devised a more practicable operation and soon placed cordotomy among the routine surgical procedures. In 1920, he reported that the optimal site for surgical section of the cord was in the upper thoracic region (3).
Additionally, Dr. Frazier, with Dr. Mills and others, reported on the surgical removal of tumors of the cerebellum, citing six cases with five recoveries, an unusual report of success at that time. His fundamental contributions to the problems of pituitary and parasellar tumors and of neoplasms of the sphenoidal ridge should not be overlooked.
In 1922, at age 52, Dr. Frazier succeeded John B. Deaver as the John Rhea Barton Professor of Surgery and was appointed chairman of the Department of Surgery at the Perelman School of Medicine. In 1925, he received an honorary degree of Doctor of Science and, in 1934, was elected a Trustee of the University (1). He was a founder-member and president of the Society of Neurological Surgeons from 1921-1923 and in 1929, he served as president of the American Neurological Association.
Dr. Frazier, known affectionately as Pop Frazier to his interns, was a tall, striking, aristocratic, sturdily built man with a ruddy complexion and piercing, keen, blue-gray eyes. He was a tireless worker and expected his students and associates to be the same.
He was known to suffer from insomnia and if he could not sleep he would call the intern at two or three in the morning and have them "pre-op" a patient for surgery in one hour. He would then operate until breakfast and then start the day's schedule.
He would not tolerate argument without fact, and consequently seemed abrupt and curt. He had a fiery temper; his rich resounding voice and commanding temperament struck fear in many colleagues as well as interns and residents, who considered him autocratic and tyrannical (2). There developed an informal organization within the university hospital known as the "Frazier Club" consisting of interns and residents whom Dr. Frazier had dismissed peremptorily from the operating room in the middle of a case. Nearly all of the experienced house officers were members.
Despite these outbursts, fundamentally, and to those who knew him more intimately, Dr. Frazier was a delightful companion, gracious, charitable, righteous, helpful and an unforgettable teacher.
Charles Harrison Frazier, with Harvey Cushing, was responsible for the development of neurosurgery in the United States. He inaugurated a dynasty of neurosurgical excellence at the University of Pennsylvania, being succeeded, in turn, by locally trained students Francis Grant (1891-1967), Robert Groff (1903-1975), and Frederick Murtagh (1917-1996) and later by Thomas W. Langfitt (1927-), Eugene S. Flamm (1937-) and M. Sean Grady (1955-). Many of his trainees went on to develop neurosurgical services and training programs elsewhere, including Alfred Adson at the Mayo Clinic, James Gardner at Western Reserve University, Stuart N. Rowe at Pittsburgh, James Watts at George Washington, Donald Munro at Harvard and Max Peet at the University of Michigan.
Dr. Francis Grant
 Dr. Francis Grant succeeded Dr. Frazier as chairman of neurosurgery in 1936, the year of Frazier's death. Temple Fay, another Frazier trainee, moved to Temple in 1929 and established the first full Department of Neurology and Neurosurgery which was a prototype of neurosurgery at Penn.
Dr. Francis Grant succeeded Dr. Frazier as chairman of neurosurgery in 1936, the year of Frazier's death. Temple Fay, another Frazier trainee, moved to Temple in 1929 and established the first full Department of Neurology and Neurosurgery which was a prototype of neurosurgery at Penn.
Dr. Grant, a born Philadelphian and graduate of Pennsylvania's School of Medicine in 1919, completed a two-year internship at the Hospital of the University of Pennsylvania before becoming a resident of Dr. Frazier's. In 1928, he was elevated to the position of Assistant Professor of Neurosurgery and in 1935 to full professor before becoming the first Charles Harrison Frazier Professor and Chairman in 1936.
Dr. Grant continued Dr. Frazier's work in developing the subtemporal operation for trigeminal neuralgia. In 1956, in the Journal of Neurosurgery, he reported 2,725 operations performed over a 30-year period, on over 2,000 patients with intracranial tumors. This paper remains an outstanding evaluation of the results of intracranial surgery for the evacuation of neoplasms.
Dr. Grant later became chairman of the American Board of Neurological Surgery, and was responsible for much of the present system of training neurosurgical specialists.
Robert Armand Groff
 Robert Armand Groff became chairman of neurosurgery in 1957. He also received his BA and MD from the University of Pennsylvania and he completed a two-year internship at the Hospital of the University of Pennsylvania. He served a one-year volunteer assistantship with Dr. Cushing in Boston and then in 1934 became an assistant to both Dr. Frazier and to Dr. Grant. He later served as an Assistant Professor of Neurosurgery at Jefferson Medical College and as Professor and Chairman of the Department of Neurosurgery at the Graduate Hospital in Philadelphia before returning to Penn.
Robert Armand Groff became chairman of neurosurgery in 1957. He also received his BA and MD from the University of Pennsylvania and he completed a two-year internship at the Hospital of the University of Pennsylvania. He served a one-year volunteer assistantship with Dr. Cushing in Boston and then in 1934 became an assistant to both Dr. Frazier and to Dr. Grant. He later served as an Assistant Professor of Neurosurgery at Jefferson Medical College and as Professor and Chairman of the Department of Neurosurgery at the Graduate Hospital in Philadelphia before returning to Penn.
Dr. Groff published over 50 scientific articles and a book entitled Manual of Diagnosis and Management of Peripheral Nerve Injuries. He was the first to develop a canine model for cerebral abscess and the first to describe, with Dr. Bernard J. Alpers, the syndrome associated with lesser wing ridge meningiomas. He is also credited, with Dr. Frederick H. Lewy, with furthering the understanding of the mechanism and treatment of the Marcus Gunn Phenomenon.
Dr. Groff retired from the chairmanship on July 1, 1968 and was succeeded by Thomas W. Langfitt.
Thomas W. Langfitt
 Dr. Langfitt is a graduate of Princeton University and the Johns Hopkins University School of Medicine where he also completed his post-graduate training in neurosurgery under Dr. A.E. Walker. He served on the faculty at the University of Pennsylvania for 25 years and held the position of chairman of neurosurgery for almost 20 years. In addition to being chairman, he served as the Vice President for Health Affairs, responsible for the university hospital, medical school, and other health professional schools.
Dr. Langfitt is a graduate of Princeton University and the Johns Hopkins University School of Medicine where he also completed his post-graduate training in neurosurgery under Dr. A.E. Walker. He served on the faculty at the University of Pennsylvania for 25 years and held the position of chairman of neurosurgery for almost 20 years. In addition to being chairman, he served as the Vice President for Health Affairs, responsible for the university hospital, medical school, and other health professional schools.
His contributions to neurosurgery were numerous including more than 200 publications. His principle interests were in the fields of head injury, intracranial pressure and cerebral blood flow and metabolism.
Eugene S. Flamm
 Eugene S. Flamm was recruited from New York University to lead the department of neurosurgery in 1988. Flamm's passion for neurosurgery began early and included two years in neurosurgery training at the National Institutes of Health as well as a challenging residency with Joseph Ransonhoff at NYU. This was followed by a fellowship in Zurich with Hugo Krayenbuhl and Professor M. Gazi Yasargil.
Eugene S. Flamm was recruited from New York University to lead the department of neurosurgery in 1988. Flamm's passion for neurosurgery began early and included two years in neurosurgery training at the National Institutes of Health as well as a challenging residency with Joseph Ransonhoff at NYU. This was followed by a fellowship in Zurich with Hugo Krayenbuhl and Professor M. Gazi Yasargil.
Dr. Flamm returned to the faculty of NYU, becoming vice-chairman and professor in the department and director of the neurosurgical research laboratories. His research interests have included cerebral vasospasm, cerebral ischemia, free radicals, and spinal cord injury for which he shared the 1990 Wakeman Award for Research in Neurosciences.
He helped establish the Penn Neurological Institute which coordinated the clinical activities of the departments of neurosurgery and neurology in order to improve delivery of patient care. In 1997, he successfully orchestrated the conversion of the division of neurosurgery to an independent department.
M. Sean Grady
 Dr. Flamm's departure in 1998 led in July 1999 to the appointment of M. Sean Grady, MD as the Charles Harrison Frazier Professor and Chairman of the Department of Neurosurgery. Following medical education at Georgetown University, Dr. Grady trained in neurosurgery with John A. Jane, MD, PhD, at the University of Virginia.
Dr. Flamm's departure in 1998 led in July 1999 to the appointment of M. Sean Grady, MD as the Charles Harrison Frazier Professor and Chairman of the Department of Neurosurgery. Following medical education at Georgetown University, Dr. Grady trained in neurosurgery with John A. Jane, MD, PhD, at the University of Virginia.
With outstanding academic training from Dr. Jane and research training in central nervous system plasticity from Oswald Steward, PhD, Dr. Grady joined Dr. Richard Winn and the faculty of the department of neurological surgery at the University of Washington in Seattle. In his 12 years there, Dr. Grady focused his efforts on research (memory dysfunction following traumatic brain injury) and clinical care (trauma, spinal disorders, vascular disorders and stereotaxis).
With the new millennium and the challenges facing health care, Dr. Grady was dedicated to ensuring that Penn Medicine continued to train neurosurgeons in the classic tradition of active participation in research, clinical care and education, so that residents would be trailblazers for academic neurosurgery.
Daniel Yoshor
 Daniel Yoshor was given the Charles Harrison Frazier Professorship in 2020. Prior to coming to Penn, he served as the Marc J. Shapiro Professor and Chair of the Department of Neurosurgery at Baylor College of Medicine. He holds a BA in philosophy from Yeshiva University and an MD degree with honors from the University of Chicago. He completed his neurosurgery residency at Baylor College of Medicine followed by fellowship training in brain tumor and epilepsy surgery at University of California, San Francisco.
Daniel Yoshor was given the Charles Harrison Frazier Professorship in 2020. Prior to coming to Penn, he served as the Marc J. Shapiro Professor and Chair of the Department of Neurosurgery at Baylor College of Medicine. He holds a BA in philosophy from Yeshiva University and an MD degree with honors from the University of Chicago. He completed his neurosurgery residency at Baylor College of Medicine followed by fellowship training in brain tumor and epilepsy surgery at University of California, San Francisco.
As a clinical neurosurgeon, Dr. Yoshor focuses on tumor and epilepsy surgery. He has one of the largest experiences in the nation in endoscopic pituitary and skull base tumor surgery. He also has extensive experience in the development and clinical implementation of novel neurotechnologies. As a neuroscientist, Dr. Yoshor is an established principal investigator with long record of NIH, DARPA, and VA Merit Award funding. Work from his laboratory has been published in leading scientific journals including Cell, Current Biology, eLife, Nature Medicine, Nature Neuroscience, Journal of Neuroscience, Neuron, and PNAS. His long-term research goals are to understand how neural activity in the brain is linked to perception and to develop a cortical visual prosthetic device to restore vision to the blind, in collaboration with a larger team of scientists, engineers, and clinicians.
Building on the groundwork put in place by Dr. Grady, Dr. Yoshor is committed to making the neurosurgery department at Penn Medicine the best in the country. He has ushered in a new era by creating divisions of four core subspecialties: Spine and Peripheral Nerve, Stereotactic and Functional, Neuro-Oncology, and Cerebrovascular and Neurointerventional. With the top clinical faculty in the field focused on their preferred area of expertise, they can now commit more time to their groundbreaking research and expose residents to a caseload that is unheard of at other institutions. Residents are now coming out of our program with a focused clinical and academic expertise and are on track to become the next generation of leaders in their respective areas.