 Up to a quarter of patients treated for thyroid cancer will experience issues with vocal tone, pitch, endurance and resonance in the months following surgery and radiation therapy. The mission of the Penn Center for Voice, Speech and Swallowing (CVSS), and its director Natasha Mirza, MD, is to restore these patients to levels of vocal function approaching their pre-cancer condition, and enabling their return to the normal interactions of daily life and work.
Up to a quarter of patients treated for thyroid cancer will experience issues with vocal tone, pitch, endurance and resonance in the months following surgery and radiation therapy. The mission of the Penn Center for Voice, Speech and Swallowing (CVSS), and its director Natasha Mirza, MD, is to restore these patients to levels of vocal function approaching their pre-cancer condition, and enabling their return to the normal interactions of daily life and work.
Nonoperative Therapy for Vocal Fold Control in the Healing Period
“The majority of people with vocal fold control issues will improve with time,” Dr. Mirza says. “In the meantime, we have many ways of helping people regain up to 90% of the voice they had prior to surgery.”
Vocal fold issues may occur because the nerve that controls the voice has been injured during surgery or by scarring in the neck muscles resulting from surgery or radiation therapy. During this time, says Dr. Mirza, many patients experience erratic and unpredictable vocal fold function and may take six months to a year to heal naturally with the assistance of voice therapy.
 At Penn, voice therapy with our dedicated speech therapists is tremendously beneficial. Voice therapy is tailored to the unique needs of the patient and consists of exercises to strengthen the vocal folds, improve breath control during speech and protect the airway during swallowing. For patients with vocal issues caused by scarring, injections of tissue-softening steroids greatly help. For some individuals with uncontrollable neck muscle spasms usually seen after radiation therapy, neuromodulators like Botulinum toxin are used to provide relief and allow the muscle time to recover and return to normal.
At Penn, voice therapy with our dedicated speech therapists is tremendously beneficial. Voice therapy is tailored to the unique needs of the patient and consists of exercises to strengthen the vocal folds, improve breath control during speech and protect the airway during swallowing. For patients with vocal issues caused by scarring, injections of tissue-softening steroids greatly help. For some individuals with uncontrollable neck muscle spasms usually seen after radiation therapy, neuromodulators like Botulinum toxin are used to provide relief and allow the muscle time to recover and return to normal.
Treating Vocal Fold Paralysis
Vocal fold paralysis after thyroid cancer surgery, although rare, is the most common iatrogenic voice disorder. The vocal folds are disposed to post-operative paralysis as a result of malignant invasion or surgical trauma to the nerves in the larynx, or voice box. These nerves control the muscles responsible for vocal fold movement and the pitch of the voice. Because the vocal folds are paired, paralysis can be either one-sided (unilateral) or two-sided (bilateral).
Persons with unilateral vocal fold paralysis are at considerable risk for aspiration pneumonia because the normal protections the vocal folds provide are compromised on one side, thereby allowing liquids and even food to go down the airway.
Patients with bilateral vocal fold paralysis are at risk of suffocation because the vocal folds are often very close together, blocking the airflow into the tracheobronchial tree, and often need a tracheostomy to bypass the area of airway narrowing.
Treatment of Unilateral Vocal Fold Paralysis: Augmentation
“Patients with unilateral injury will have noticeable vocal fatigue, loss of projection, difficulty talking with background noise, limited pitch, a lack of vocal endurance and micro-aspiration (minor intake of saliva and fluids) during the day.” says Dr. Mirza. “It becomes a quality of life issue. They feel as though they’re not quite what they were.” Professional voice users more often notice these changes. These are individuals who use their voices as part of their profession like attorneys or singers.
 Treatment for these patients often begins with augmentation using injectable synthetic materials that hold the paralyzed vocal fold in a desired position to optimize function. This can be performed early in the post-operative period – allowing time for natural recovery of function – and is often accompanied by voice therapy.
Treatment for these patients often begins with augmentation using injectable synthetic materials that hold the paralyzed vocal fold in a desired position to optimize function. This can be performed early in the post-operative period – allowing time for natural recovery of function – and is often accompanied by voice therapy.
“Augmentation allows for quicker return to normal life for at least 50% of patients presenting with voice complaints,” says Dr. Mirza. “and Penn speech therapists can additionally help these patients with their voice through improved breathing techniques and other simple techniques such as a change in work schedule and taking a break from work until they’re in a better place with cancer care and voice rehabilitation.”
Augmentation with injectables is a temporary remedy however, and the injectable is eventually resorbed. If a patient’s voice has not recovered within the normal healing period despite injectables treatment and voice therapy, the Penn team will use advanced diagnostics to determine the cause. If these studies determine that nerve recovery is unlikely to occur, then the team discusses permanent solutions with the patient.
Surgical Options for Unilateral Vocal Fold Paralysis
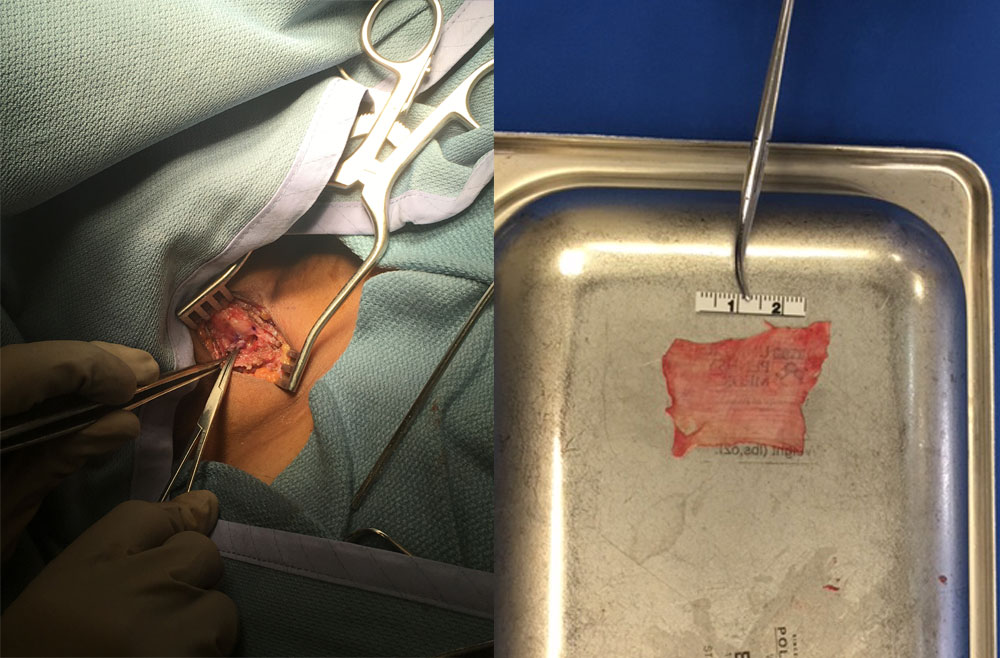 Fascia Lata graft
Fascia Lata graftMedialization thyroplasty is considered the gold standard treatment for unilateral vocal fold paralysis. This treatment involves medializing the paralyzed vocal folds with a permanent implant that is positioned to achieve the desired vocal quality and function.
Fortunately for Penn patients, we are able to provide an advanced evolution of this treatment – medialization thyroplasty with autografts such as tensor fascia lata graft.
“Traditional medialization thyroplasty is a static way of replacing the dynamic function of the vocal folds,” Dr. Mirza says. This novel technique involving an autograft, developed by Dr. Mirza and her team at Penn Medicine, allows for a static medialization while also producing excellent post-operative voice outcomes and reducing the risk of extrusion and other post-surgical complications common to areas that have been exposed to radiation.
“We developed the fascia lata thyroplasty technique at Penn Medicine so that permanent vocal fold medialization could be achieved using the patient’s native tissue, which decreases the likelihood of implant rejection or wound breakdown,” Dr. Mirza explains.
Surgical Treatment of Bilateral Vocal Fold Paralysis
At Penn, patients with bilateral vocal fold paralysis needing a tracheostomy may receive a laser endoscopic partial cordectomy to ensure that the airway is adequate and the valve is open enough for the tracheotomy to be removed.
 A minimally invasive procedure, endoscopic laser cordectomy is used to cut away a small portion of the posterior vocal fold to create an opening sufficient to result in a functional voice, yet not so large that it results in increased aspiration risk. Laser cordectomy is highly precise and associated with significant improvement in breathing. Partial laser cordectomy is a differentiating factor for medical centers treating vocal fold paralysis,” Dr. Mirza says. “Cost can be a prohibitive factor for hospitals considering laser surgery, despite the fact that it greatly enhances the safety and accuracy of treatment.”
A minimally invasive procedure, endoscopic laser cordectomy is used to cut away a small portion of the posterior vocal fold to create an opening sufficient to result in a functional voice, yet not so large that it results in increased aspiration risk. Laser cordectomy is highly precise and associated with significant improvement in breathing. Partial laser cordectomy is a differentiating factor for medical centers treating vocal fold paralysis,” Dr. Mirza says. “Cost can be a prohibitive factor for hospitals considering laser surgery, despite the fact that it greatly enhances the safety and accuracy of treatment.”
Long-Term Rehabilitation: Speech Therapy
Knowing that effective treatment doesn’t end following surgery, the Penn Speech Language Pathology specialists, and referring physicians in the community enter a long-term collaborative effort to provide support that enables patients to return to their daily life as close as possible to their pre-treatment level. Among the therapies embraced by the Center is voice restoration, with individualized vocal exercises and counseling.
“The speech pathologists are primarily teaching patients not to overstrain their voices and to breathe in a way that will maximize their voice,” says Dr. Mirza. Moreover, for patients with vocal cord injury at risk of aspiration, speech therapy specialists offer techniques (head turns, chin tucks, alterations in diet) that minimize risk and optimize control to give patients a safer swallow.
Through the coordination of speech therapy and surgical interventions, Penn is able to provide patients the best chance for voice preservation and restoration so that they can return to their normal life.