Mrs. T, 39-year-old female, never-smoker, with a history of squamous cell carcinoma in situ of the right true vocal cord, longstanding Crohn's disease, and gastroesophageal reflux, presented with a cough and sore throat. A prior right vocal cord lesion with a pathology consistent with SCC in situ with negative margins, had been treated with microlaryngoscopy and KTP laser excision 7 months earlier at another institution.
Mrs. T’s Crohn’s disease was difficult to control, with oral involvement and prior requirement for multiple immunosuppressants and steroids, including (most recently) the systemic biologic ustekinumab (Stelara). Her Penn gastroenterologist planned to switch her to vedolizumab (Entyvio) in place of ustekinumab given ongoing uncontrolled GI symptoms and the presence of the head and neck neoplasm. Vedolizumab is a more gastrointestinal-selective agent, with less systemic immunosuppression.
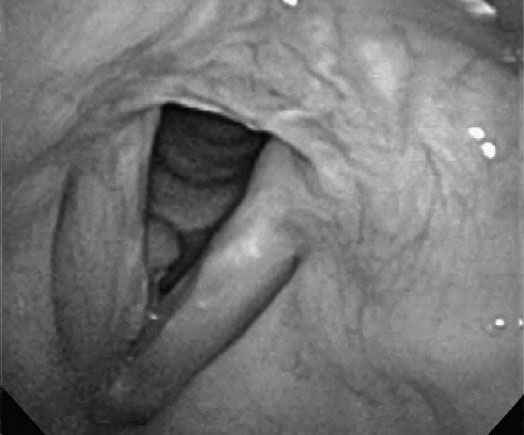 Figure 1: Photograph of patient's right vocal cord demonstrating squamous cell carcinoma.
Figure 1: Photograph of patient's right vocal cord demonstrating squamous cell carcinoma.
At presentation, Mrs. T reported a number of laryngeal symptoms including constant cough, hoarseness, and sore throat, without shortness of breath. On nasopharyngolaryngoscopy, a mass of the right anterior/mid true cord was observed (Fig 1). The entire vocal fold was noted to be edematous and erythematous, but vocal cord mobility was normal. There were no palpable cervical lymph nodes.
Mrs. T was counseled on the need for tissue biopsy of the concerning vocal cord lesion. Microdirect laryngoscopy with biopsy of the right vocal cord mass was performed in late January 2020. The lesion involved the right anterior vocal cord without involvement of the anterior commissure, very limited involvement of the inferior aspect of the vocal cord and suspicion for possible early infraglottic extension, and was noted to be partly submucosal, very firm, and adherent to the underlying muscle/ligament. Pathology was positive for invasive, well-differentiated, keratinizing SCC. Mrs. T was therefore diagnosed with a stage I (cT1aN0M0) SCC of the right vocal fold.
At this point, COVID-19 had entered our institution. Standard-of-care options would normally include open or endoscopic cordectomy or definitive radiotherapy. Radiation oncology favored primary surgical resection over radiotherapy given the risk of increased radiation toxicity in a patient with active Crohn's disease with oral cavity involvement, the risk of exposure to SARS-CoV-2 from other patients and health care providers during a typical 28-fraction (6 week) course of radiotherapy, which would have corresponded to the predicted peak surge in COVID-19 cases in our region, and her young age and hypothetical risk of secondary malignancy.
After discussion of the risks and benefits of the different options with Mrs. T and in collaboration with our multidisciplinary team, she decided to undergo laser cordectomy. It was felt that an outpatient procedure was preferable, with avoidance of open partial laryngectomy with imbrication and tracheostomy, and that the procedure should be done with the sharp (cold) technique instead of laser to minimize aerosolization.
At the time of surgery, the tumor was found to be considerably more extensive in terms of infraglottic spread than had been anticipated, the likely result of progression over the very short interval since the original diagnosis.
Mrs. T was discharged following surgery. Final pathology revealed a keratinizing, well-differentiated, invasive squamous cell carcinoma of the right vocal cord with negative, but close margins, pathologically staged as T2a. Tumor board consensus was to follow Mrs. T by telemedicine for the next several weeks and have her return for an in-person visit after the anticipated viral infection “surge” in our community. If at this time a recurrence was found, radiotherapy or supracricoid partial laryngectomy would be considered.
To date, Mrs. T is recovering well postoperatively, with her care being coordinated via telemedicine.
This case appeared in a slightly different form in Head & Neck 2020;42:1131–1136.
Discussion
The COVID-19 pandemic has complicated the management of head and neck cancers, particularly for patients with underlying immunosuppressive disorders. The imposition of protective precautions has tasked head and neck oncologists with the need to temper the risks of cancer progression while managing the risks implicit in increased susceptibility to life-threatening complications from viral exposure.
Necessary head and neck cancer surgeries continued at the Department of Otorhinolaryngology-Head and Neck Surgery in the days and weeks after the onset of the COVID pandemic in Philadelphia. As the following case reports demonstrate, the treatment of these complex patients required not only depth of experience, but an evolving algorithm defined by on the spot innovation, rapid decision-making and truncated response times.
When originally published in a slightly different format, the three cases that follow were intended at publication to provide guidance to clinicians struggling with how to best counsel and manage this unique subset of patients under the difficult circumstances of the COVID era.
Read other complex cases for head and neck cancer treatment during COVID
Management of Complex Head and Neck Cancers in the COVID Era – Case #1
Management of Complex Head and Neck Cancers in the COVID Era – Case #2