 Despite the quality of care received at initial fracture treatment, as many as 20% of fractures may result in a malunion or nonunion. The causes of these healing defects are often difficult to identify and complex to treat, requiring specialized training and resources to correct.
Despite the quality of care received at initial fracture treatment, as many as 20% of fractures may result in a malunion or nonunion. The causes of these healing defects are often difficult to identify and complex to treat, requiring specialized training and resources to correct.
Under the guidance of Penn surgeons Samir Mehta, MD, Stephen Kovach, MD, and L. Scott Levin, MD, the Penn Orthoplastic Limb Salvage Center (POLSC) has developed an algorithm for the management of nonunion and malunion fractures of the limbs. Nonunion and malunion fractures are identified with defective healing: nonunion describes the failure of a fractured bone to heal and mend after an extended period of time; malunion refers to a fracture that has healed in a deformed position, or with shortening or rotation of the limb.
Malunion and nonunion defects are caused by complications imposed upon the original injury, so the treatment approach to these complex injuries differs significantly from common fractures.
To address these issues, the specialists at the Center create and coordinate a systematic, individualized plan of care to target the specific cause of injury and restore the patient to optimal function.
 Malunion
Malunion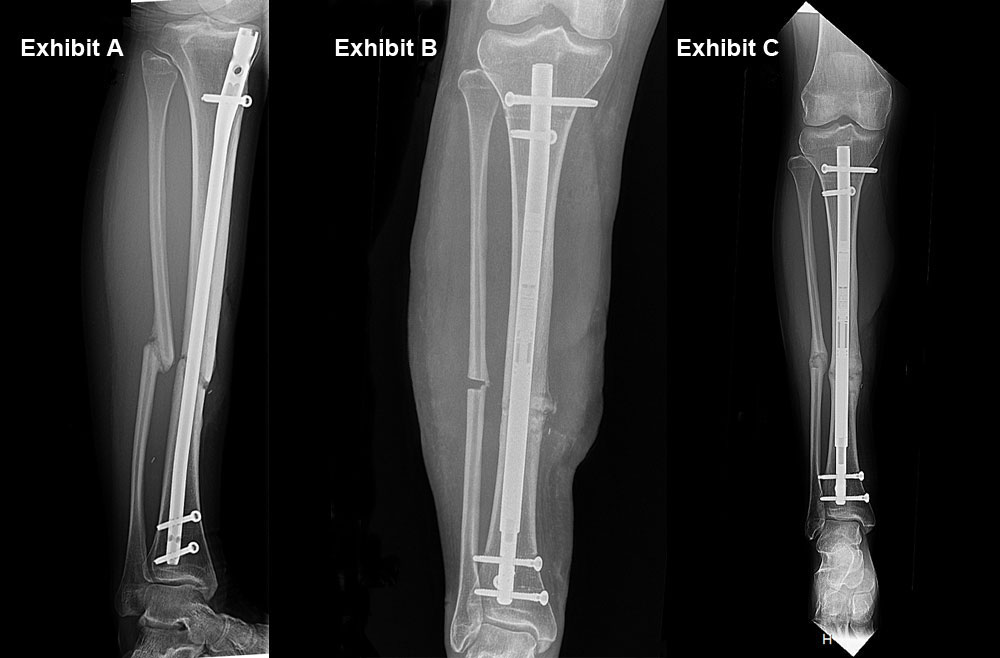 Nonunion: Infected tibia nonunion (Exhibit A). Acute shortening of tibia (Exhibit B). Lengthened leg (Exhibit C).
Nonunion: Infected tibia nonunion (Exhibit A). Acute shortening of tibia (Exhibit B). Lengthened leg (Exhibit C).
Fracture Factor #1: Infection
Eradication of infection is often the first step. Osteomyelitis (bone infection) is a cause of healing complications, bone death, hardware failure and, in severe circumstances, sepsis and amputation. Even low grade infections, which can evade detection in extremity injuries using traditional methods, can stifle healing.
“Infection often happens because the soft tissue envelope hasn’t been restored,” Dr. Mehta says. “Among the things that sets us apart as a program is that we’re blessed with skilled plastic surgeons capable of undertaking complex soft tissue repairs of the extremities.”
Infection must be managed through suppression or clearance before reconstruction can occur, an endeavor involving a multi-step process at the Center that includes antibiotics, debridement of the affected bone and soft tissue, wound closure and possibly removing previous hardware, a step that eliminates bacteria adhering to the metal and external access to the wound site.
Once infection is cleared, other morbidities or concerns impeding healing and restoration for malunion or nonunion may be addressed. Penn surgeons also use antibiotic-laced bone cement during subsequent fracture reconstruction as an additional measure to prevent the infection from returning.
Fracture Factor #2: Inadequate Blood Flow
 Inadequate blood flow, if present, is a cause of bone tissue breakdown and bone death (osteonecrosis). When inadequate blood supply to the bone is suspected, a CT or SPECT scan can be initiated to determine the presence of dead bone, but is not always reliable.
Inadequate blood flow, if present, is a cause of bone tissue breakdown and bone death (osteonecrosis). When inadequate blood supply to the bone is suspected, a CT or SPECT scan can be initiated to determine the presence of dead bone, but is not always reliable.
Treatment of osteonecrosis at the Center typically involves excoriation to remove dead bone at the nonunion, followed by microsurgery (an integral skillset for surgeons at the Center), vascularized or nonvascularized bone grafts and osteogenic or revascularization interventions to restore living bone and blood flow to the site of injury.
If the amount of affected bone removed results in a disproportion in length, advanced limb lengthening procedures are put in place. The Limb Lengthening Program at Penn has highly-skilled specialists who can correct and improve limb length inequalities using an advanced, modern technique offered at only a few centers in the country. Compared to traditional limb lengthening technology which required a large external fixation framework around the affected limb including several pins that penetrate the tissue on either side of the defect, this novel process is much easier for the patient and carries much lower risk for infection. While it may not be amenable to all patients, when possible, advanced options are utilized.
The lengthening procedure involves a surgical break in the femur and/or tibia through small incisions in the affected leg. A magnetic lengthening rod is then inserted into the bone ends. The lengthening rod houses a tiny geared mechanism controlled by an external magnet. When the patient applies an external magnet over the rod, the gears in the mechanism rotate to gradually increase the length of the limb, typically between ½ millimeter a day. The amount of time for the lengthening depends on the amount of distance needed. As the bones lengthen over time, muscle, tendon, skin, and arteries also respond and grow.
Fracture Factor #3: Biomechanics
 Biomechanical failure can be caused by any of a number of incidents that prime the fracture for instability and consequent hardware failure, resulting in malunion and nonunion.
Biomechanical failure can be caused by any of a number of incidents that prime the fracture for instability and consequent hardware failure, resulting in malunion and nonunion.
“Instability at the fracture site months after injury is a clear sign of biomechanical failure,” says Dr. Mehta. “The first step, then, is to remove the hardware, address any issues at the fracture site, then allow some time for the bones to regain strength by providing stability.”
During this interval, POLSC surgeons develop a fixation strategy to ensure stability in the subsequent repair, a plan that begins with an evaluation of the patient’s musculoskeletal structure and an effort to determine the cause of original hardware failure. A blueprint for fixation and follow-up care is then created and put into action.
Depending upon the mechanical circumstances at the fracture, surgical fixation proceeds. A traditional rigid construct can be used as well as an innovative dynamic (flexible) implant. Comprised usually of screws and plates, dynamic implants are used to treat fractures at the distal femur and other locations that require dynamic stress to heal optimally.
Biomechanics of another sort may play a role in malunion, where hardware issues or bone alignment during healing may result in limited functional capability or capacity.
“A malunion typically occurs when a fracture has not been aligned and stabilized in a way that optimizes fracture healing,” Dr. Mehta explains. “When this results in rotation or shortening of the limb, it becomes a mechanical issue that interferes with normal function.” The standard repair for malunion is to reset the bone and refit the hardware in such a way that proper healing can take place.
“One of the advantages at Penn is our capacity to recognize the potential for malunion in the way a bone is responding to fixation,” Dr. Mehta says of the subtleties of bone healing and repair. “This is achieved by monitoring bone and soft tissue coverage in the immediate wake of repair.”
Fracture Factor #4: Patient Biology
 Biology is also an important element in healing, and patients entering the POLSC undergo a series of metabolic panels and other lab evaluations to gauge the body’s capacity to repair bone. Factors that influence body chemistry, metabolism and immune response, including patient lifestyle and medical history, also contribute to a patient’s healing potential.
Biology is also an important element in healing, and patients entering the POLSC undergo a series of metabolic panels and other lab evaluations to gauge the body’s capacity to repair bone. Factors that influence body chemistry, metabolism and immune response, including patient lifestyle and medical history, also contribute to a patient’s healing potential.
“We want to know whether a patient smokes or is taking certain medications which negatively impact bone healing, and we look at past episodes of disease, particularly endovascular and metabolic disorders,” says Dr. Mehta. The result of these investigations will determine the measures undertaken prior to repair, including patient counseling, medical interventions for hormonal and nutritional deficits and consults with specialists whose insights will determine direction before and after malunion and nonunion repair.
Referring to the Center for Malunions and Nonunions
The Penn Orthoplastic Limb Salvage Center (POLSC) is a combined plastic surgery and orthopedic treatment program for patients with complex limb needs like malunion and nonunion fracture care, along with osteomyelitis and soft tissue management after fracture or injury. The center serves as a resource of support to providers who may need assistance managing complex patients that may come under their care.
To refer a patient to the Center, call 215-294-9625, who will coordinate your patient’s care at our Penn Orthoplastic Limb Salvage Center. For urgent or emergent management of a patient, please call 215-615-6978 and you will be directly speaking with a Penn Orthoplastic Limb Salvage Center surgeon.